Key Integration Challenges with Legacy Healthcare Systems
Discover key challenges of integrating legacy healthcare systems and learn practical solutions to streamline workflows and improve patient care.
Research by Mulesoft and Deloitte revealed that enterprises use an average of 976 applications. Only 28% of these are integrated.
While the number may sound too big to be true for most businesses, here's what is true:
Most businesses today are using more applications and tools than ever before.
While the goal of using these apps and tools is to make things simpler, it actually complicates things. Different systems often don't speak to each other. The data gets trapped in silos. Employees get burdened with too many apps to check. And general chaos ensues.
For healthcare businesses, too many apps become even more of a problem because of the legacy systems in place.
Healthcare today is more complicated than ever before. Medical professionals are juggling patient care, administrative tasks, regulatory compliance, and now, technology.
Software solutions are the backbone of modern healthcare. They help:
Streamline patient data
Reduce redundancy
Enhance operational efficiency
But this is all easier said than done. The very foundation you rely on - your legacy systems - often turns into the biggest roadblock.
Now this might feel frustrating. After all, these systems have served you well for years. They’re familiar, dependable, and deeply rooted in your organization. But they aren't built for the modern integrations that you now need.
That's why it is common to face many challenges in legacy healthcare system integrations.
What are those challenges?
How to overcome them?
Find answers to all these questions in this blog right here. Read on.
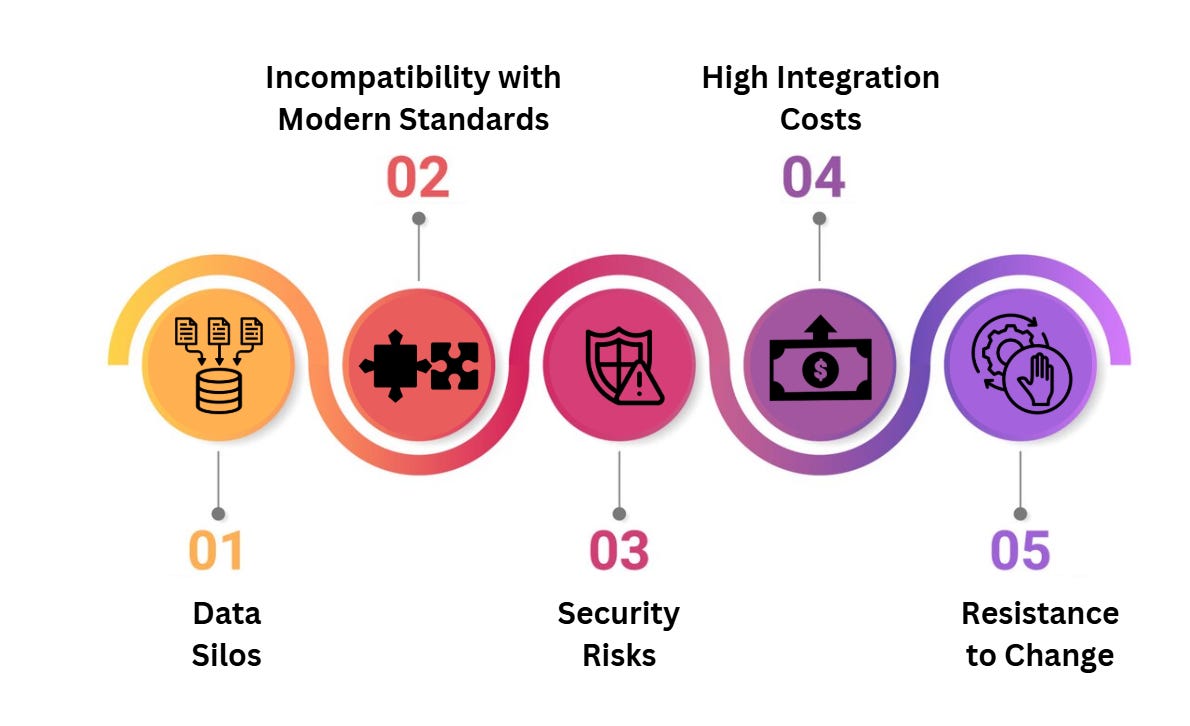
5 Key Challenges of Legacy Healthcare System Integrations
1. Data Silos
Legacy systems are notorious for locking up data in separate silos. Each department might have its own software, and they rarely talk to each other. This creates a fragmented view of patient information, making it hard to deliver coordinated care.
How to Fix This:
Start with a thorough audit of your systems. Identify what data is stored where and how it’s being used.
Invest in middleware solutions that act as a bridge between legacy systems and modern applications.
Standardize data formats to ensure consistency across platforms.
This step alone can break down barriers and help your team see the bigger picture.
2. Incompatibility with Modern Standards
Most legacy systems weren’t built to comply with modern interoperability standards like HL7 or FHIR. This makes it challenging to exchange data with newer healthcare applications.
How to Fix This:
Work with integration platforms that specialize in converting legacy data into modern formats.
Collaborate with vendors to update existing systems where possible.
Implement APIs to facilitate communication between old and new systems.
This ensures your data flows smoothly without requiring a complete system overhaul.
3. Security Risks
Security isn’t optional. It’s non-negotiable, especially in healthcare.
But let’s face it—legacy systems weren’t designed with today’s cybersecurity threats in mind. Integrating them with modern solutions can expose vulnerabilities, putting sensitive patient data at risk.
How to Fix This:
Conduct a security assessment before starting any integration project.
Layer your legacy systems with updated security protocols like encryption and multi-factor authentication.
Monitor data flows continuously to detect and mitigate risks in real-time.
4. High Integration Costs
Integrating legacy systems can be expensive. Between custom development, middleware, and consulting fees, costs can quickly spiral out of control.
How to Fix This:
Prioritize integrations based on ROI. Start with systems that will deliver the biggest impact.
Consider phased integration to spread costs over time.
Leverage open-source tools where possible to reduce licensing fees.
Important: Cost management doesn’t mean cutting corners. It means being smart about where you invest.
5. Resistance to Change
Let’s be real—people are creatures of habit. Your team might resist changes to systems they’ve been using for years. Add integration challenges on top of that, and you’ve got a recipe for pushback.
How to Fix This:
Involve your team early in the integration process. Get their feedback and address their concerns.
Provide training to help them understand the new workflows.
Show them the benefits in real terms, like how it will save time or reduce errors.
When people feel heard and supported, they’re more likely to embrace change.
Getting Started With A Professional HealthTech Partner
Here’s an important piece of truth: integrating legacy systems isn’t something you should tackle alone. It’s complex, time-consuming, and often overwhelming. That’s where a professional healthtech company comes in.
A good partner will:
Analyze your existing systems and design a roadmap tailored to your needs.
Use the latest tools and techniques to ensure seamless integration.
Train your staff and provide ongoing support to keep everything running smoothly.
Most importantly, they’ll help you focus on what really matters—delivering exceptional care to your patients.
Let’s Make This Easier for You
If you’ve been nodding along, thinking, “This is exactly what we’re dealing with,” know that you’re not alone. These challenges are common, but they’re also solvable. With the right approach and the right partner, you can integrate your systems without losing your sanity—or your budget.
So, why not take the first step? Start by identifying where your integration pain points are. And if you’re ready to make this process smoother and stress-free, reach out to a professional healthtech company. We’ve done this before, and they know how to make it work for you.
Because at the end of the day, integrated systems aren’t just about technology—they’re about better patient outcomes, happier teams, and a more efficient organization.
Schedule a call with our HealthTech experts to get a headstart today!